In this module, you will learn about the following topics:
1) Anatomy of the knee
The knee joint is is the connection between the upper leg and the lower leg.
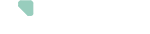
The knee joint is formed by 3 bones:
- the thigh bone (femur)
- the shin bone (tibia)
- the patella (knee cap)
The knee joint has 3 compartments:
- the medial compartment (inner side of the knee joint)
- the lateral compartment (the outer side of the knee joint)
- the patella-femoral compartment (between the knee cap and the thigh bone).
The knee cartilage
At the end of these bones where the joint articulates, the bone is covered with cartilage. This cartilage helps to make the joint surfaces slide more easily over each other so that one can move smoothly and painlessly in the joint.
Two C-shaped pieces of cartilage called the medial and lateral meniscus act as shock absorbers between the femur and tibia.
The knee ligaments
Ligaments join the knee bones and provide stability to the knee.
2) What is knee osteoarthritis?
In some cases, such as with osteoarthritis, the cartilage that helps the bones to move smoothly may be damaged. In osteoarthritis, the cartilage becomes thinner and softer.
The degeneration of cartilage can be a natural process but it can be accelerated by various factors such as long-term inflammation in the knee, previous injuries, or surgeries such as the repair of the cruciate ligaments of the knee. Osteoarthritis in the knee can be localized in one or more compartments of the knee.
Due to the damage to the cartilage itself, changes can also take place in the bone just below the cartilage. For example, bony lumps, also called osteophytes, can form at the edge of the joint. The joint capsule, the tendons and the muscles around the joint can become irritated. This can lead to a decrease of function of the knee and can be accompanied by pain.

3) Knee replacement surgery
The operation
The surgery will restore the optimal gliding movement between the joint surfaces, and reduce pain and mobility restrictions. To do this, the surgeon will remove the damaged joint surfaces and replace them with the prosthesis.
In recent years, the number of knee prostheses has increased steadily. The placement of a knee prosthesis is a surgery that has become common in recent years. This increase in the number of cases also leads to a better mastery of the entire protocol, surgical and material innovations. This evolution allows for faster post-operative recovery and make it easier for patients to resume their activities.
The surgery approach
Depending on your type of surgery, your body type, and musculature, the surgeon will have to make an incision of about 10 and 15 cm either on the front of the knee or an incision more towards the inner part of the knee.
The prosthesis
A prosthesis is made of high-tech material:
- Chrome/Cobalt alloy or titanium for the parts that are fixed to the bone
- Polyethylene (a very strong and wear resistant plastic) central piece that facilitates the gliding movement
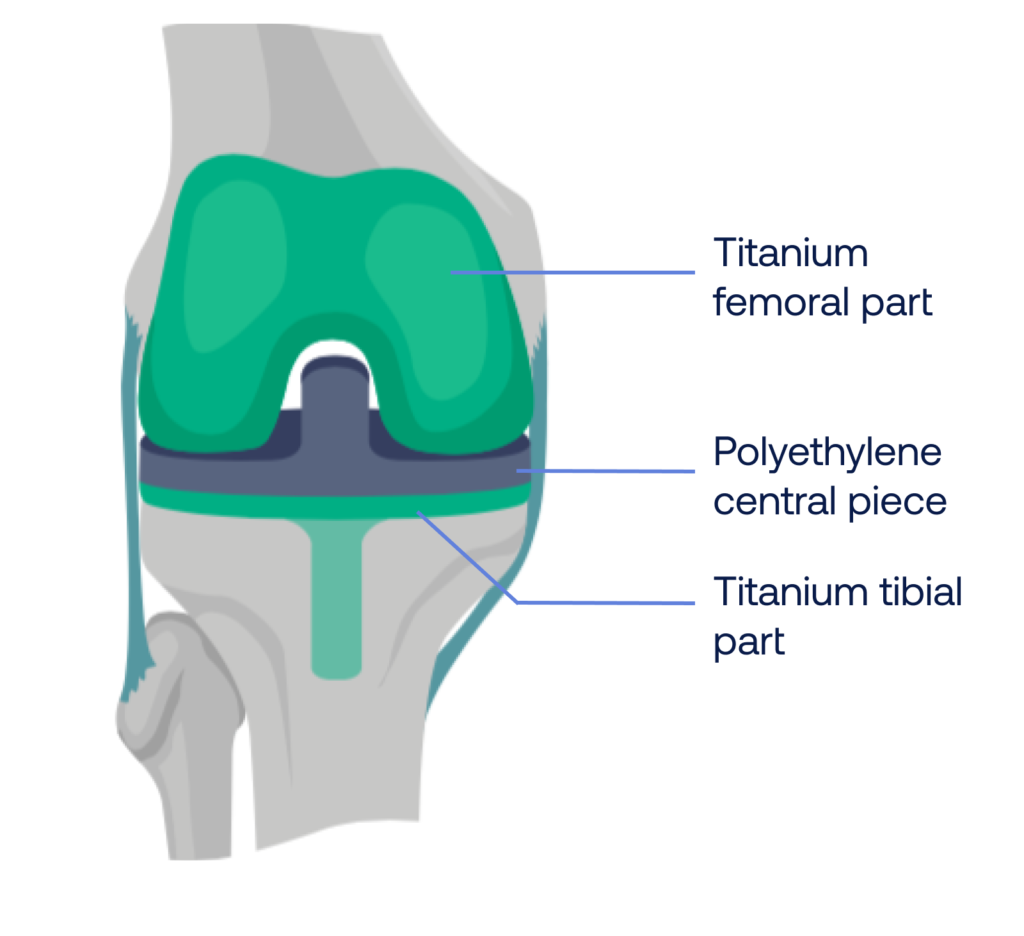
The knee prosthesis can be cemented or uncemented.
Depending on where the osteoarthritis is located, your surgeon might opt for a bicompartimental (total) knee replacement or an unicompartimental knee replacement.
In a total knee replacement, both the medial and lateral compartment are replaced. In some case, the cartilage behind your patella or knee cap will also be replaced depending on the surgeon’s preference.
In an uni-compartimental knee replacement, either the medial or the lateral compartment is replaced. However, if both compartments show signs of osteoarthritis, a total knee replacement will be advised to avoid a second surgery.
The final result one year after the operation is the same for the various surgery approaches. It is therefore recommended to choose the surgery approach in which your doctor is specialized. Your surgeon will always consider your personal needs and complaints when making the decision for surgery.
The goal of knee replacement surgery is to:
- regain mobility (usually between 120° and 135°, but this will also depend on your pre-operative mobility),
- decrease complaints such as stiffness and/or pain, and
- improve your quality of life and walking activities