In this module, you will learn about the following aspects:
1) Anatomy and cause of osteoarthritis
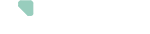
The hip joint is the connection between the femur bone (femoral head) and the pelvis (acetabulum). Cartilage lies on the joint surface of the femoral head and acetabulum. This cartilage helps to absorb shocks and to make the joint surfaces slide more easily over each other so that one can move smoothly and painlessly in the joint. The joint is surrounded by a capsule and a set of muscles and ligaments connecting the femur and the pelvic bone. The joint capsule is a flexible and resistant fibrous envelope that plays an important role in the stability of the hip joint.
2) What is osteoarthritis
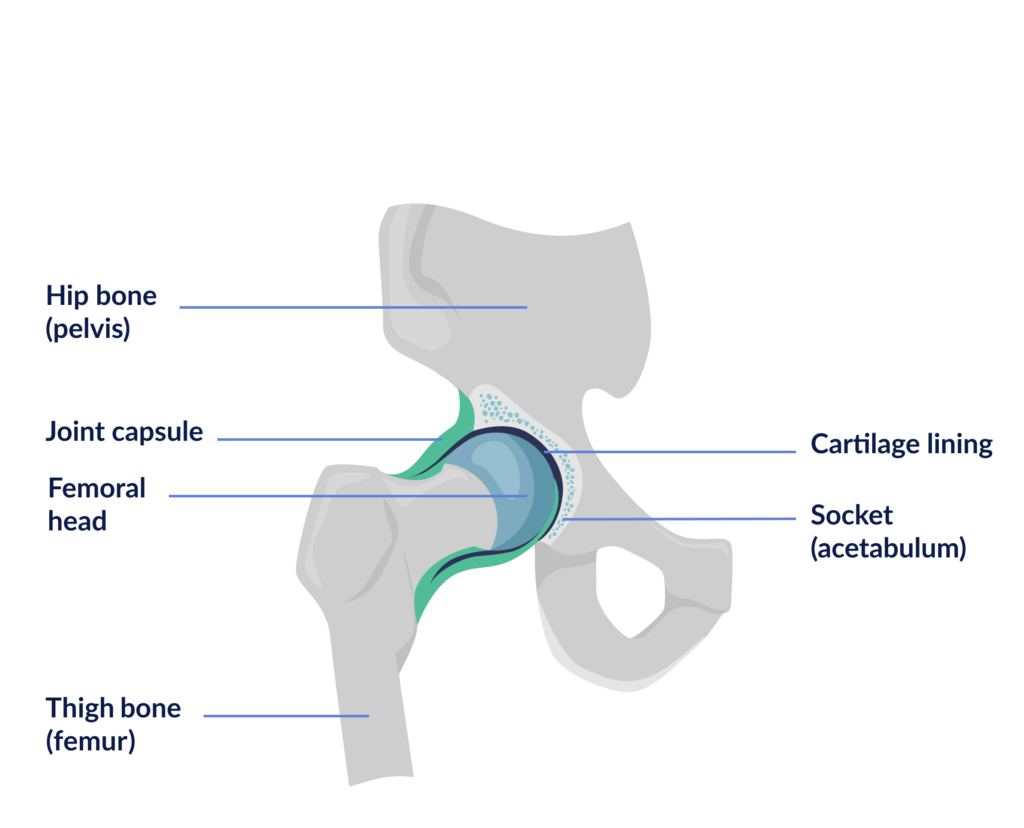
In some cases, such as with osteoarthritis, the cartilage that helps to move smoothly may be damaged. In osteoarthritis, the cartilage becomes thinner and softer.
In addition to the damage to the cartilage itself, changes can also take place in the bone just below the cartilage. For example, bony lumps, also called osteophytes, can form at the edge of the joint. The joint capsule, the tendons and the muscles around the joint can also sometimes suffer from osteoarthritis. This can lead to limitation of movement in the hip and can be accompanied by pain.
Osteoarthritis is more common in people over 65, people who are overweight or people who have suffered damage to the joint in the past due to, for example, a fracture. There is also a hereditary component in osteoarthritis. Osteoarthritis is a degenerative condition and that is why it is sometimes also referred to as ‘wear and tear’ of the joint. People with osteoarthritis of the hip joint often experience complaints at the hip for a longer period of time before taking the step to consult an orthopaedic surgeon.
Another reason that the bone or cartilage of the femoral head may be damaged is avascular necrosis. In avascular necrosis, the blood supply is temporarily or permanently reduced, causing the bone structure to change and losing its carrying capacity. However, avascular necrosis is much less common than osteoarthritis. Avascular necrosis usually also develops more quickly, so complaints can evolve more rapidly and an operation might be required sooner.
3) The operation, the prothesis and surgery approach
The operation
Hip replacement surgery has become a standard operation in recent decades with good results. More than 25,000 hip prostheses were placed in Belgium in 2019.
A hip prosthesis is recommended by the surgeon when the complaints limit a patient’s daily activities or mobility too much. On X-ray, it is usually clearly visible whether the cartilage is damaged and whether surgery is required.
During your operation, the surgeon will open the skin and move the muscular, nervous and tendinous elements. He will open the joint capsule and intentionally dislocates the hip. He will then remove the damaged femoral head and acetabulum and place the prosthesis. Once the prosthesis is in place, the capsule is closed, the displaced peri-articular elements are put back in place and the surgeon closes the wound.
This operation will restore the optimal gliding movement between the 2 bones, allowing patients to move more smoothly and pain-free.
The prothesis
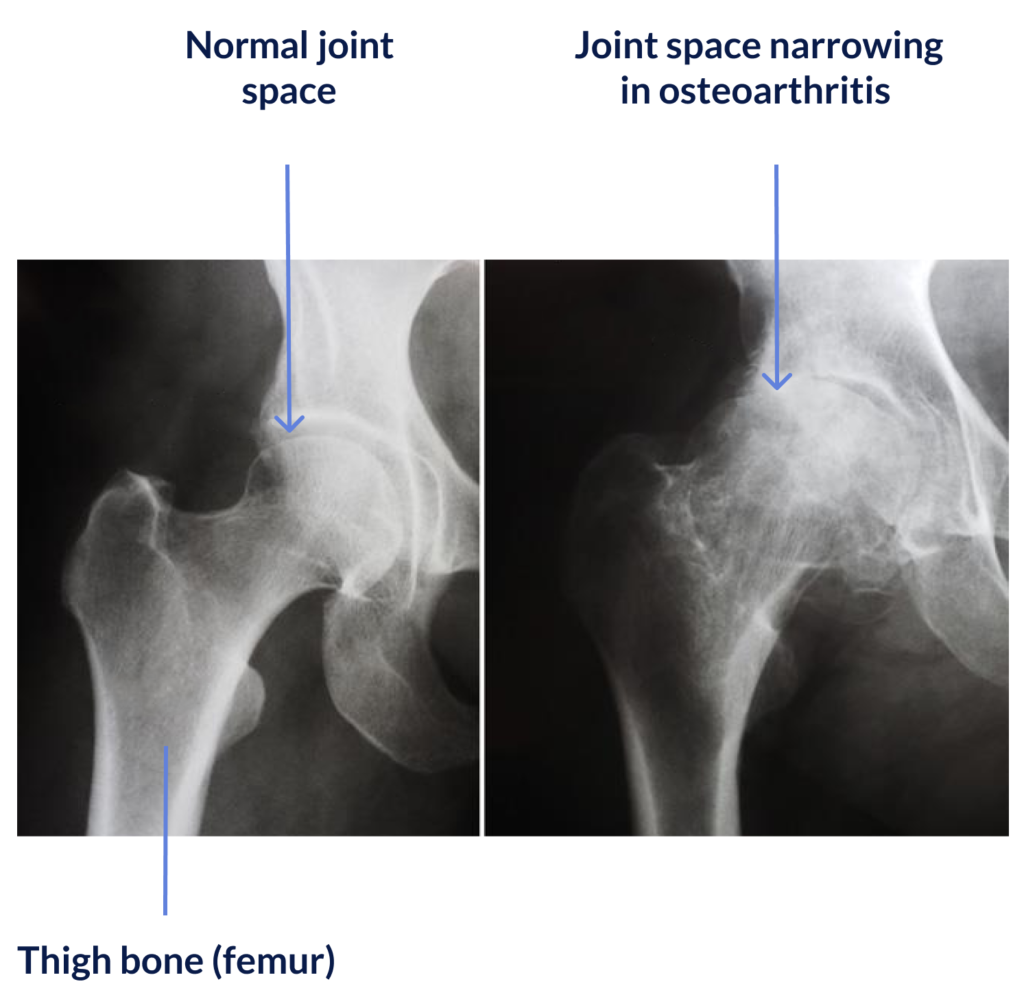
The prosthesis you will receive consists of:
- A stem with head that is in the thigh bone (femur) that replaces the hip head
- A cup that replaces the acetabulum
- Lining that replaces the cartilage
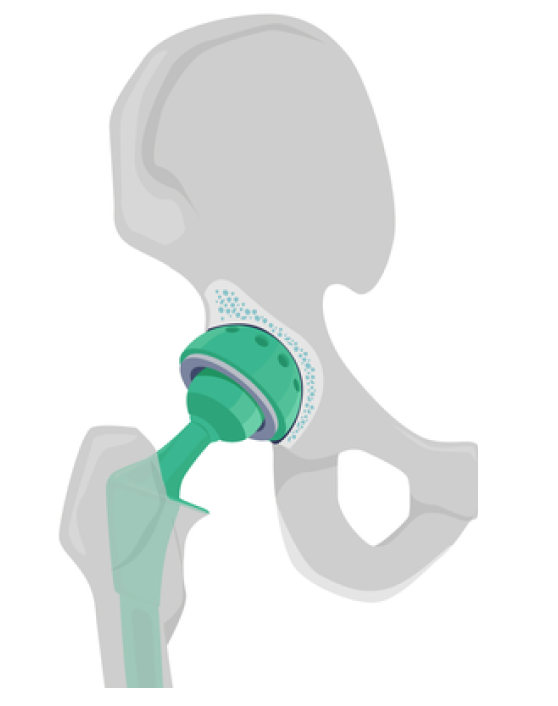
The parts that have to articulate are made of ceramic so that they slide smoothly over each other. The parts that are fitted into the bone are usually made of titanium. To ensure proper implantation of the prosthesis, the titanium surfaces are coated with a substance that activates bone healing (hydroxoapatite).
Ingrowth or consolidation takes about 6 weeks. When the consolidation is complete, the titanium and prosthesis are thus firmly integrated into your bone.
The surgery approach
Depending on your operation and various clinical parameters, the surgeon can choose between different access routes to the joint: the anterior (close to the groin), anterolateral (at the side) or posterolateral (at the buttocks) approach.
If possible, the approach that will have the least impact on your rehabilitation is chosen. This will be referred to as “minimally invasive“. The naming refers to the small size of the wound and the fact that the surgeon does not cut any muscles, but simply slides them aside during the operation. This allows for early mobilization and faster rehabilitation than before.
The final result one year after the operation is the same for the various surgery approaches. It is therefore recommended to choose the surgery approach in which your doctor is specialized.